E. Alexiev, K. Guirov, B. Guirova, A. Mihova, E. Titianova
Neurosonology and Cerebral Hemodynamics 10, 2014:15–18
| TITLE | Clinical, Intraoperative and Multimodal Ultrasound Imaging Study of Facial Melanoma |
| AUTHORS | E. Alexiev, K. Guirov, B. Guirova, A. Mihova, E. Titianova |
| PUBL. DATE | May 2014 |
| SOURCE | Neurosonology and Cerebral Hemodynamics 10, 2014:15–18 |
| TYPE | Periodic scientific journal |
| ABSTRACT |
Objective: To demonstrate the diagnostic abilities of multimodal ultrasound imaging and its correlation to clinical, intraoperative, histological and CT imaging in a rare case of facial malignant melanoma. |
| KEY WORDS |
facial melanoma, ultrasound imaging |
Melanoma is a malignant neoplasm of melanocytic origin, which arises from benign melanocytic lesions or de novo from melanocytes within otherwise normal skin or mucosa. Although most melanomas are on the skin, they may develop at any site where melanocytes are present [7].
Different risk factors play role in the etiopathogenesis of the disease with the leading significance of hereditary predisposition, individual’s phenotype, ultraviolet radiation and dysplastic congenital melanocytic nevi [1]. Four clinicopathologic types of melanoma have been described – superficial spreading, nodular, lentigo maligna and acral lentiginous melanoma [4].
Melanoma shows two-dimensional pattern of growth – with radial and vertical growth phase [8]. In the early stages the radial growth phase predominates in superficial spreading, lentigo maligna and acral lentiginous melanoma. In these lesions malignant melanocytes tend to spread horizontally through the basal layer of the epidermis. The vertical growth phase begins when the malignant cells eventually invade the underlying connective tissue. In nodular melanoma the vertical growth phase is predominant and the radial growth phase is very short or non-existent.
Criteria for early diagnosis of malignant melanoma are summarized by the American Academy of Dermatology in the ABCDE system: A (Asymmetry)=asymmetry of the lesion; B (Border)=irregular edge; C (Color)=uneven pigmentation; D (Diameter)=diameter more than 6 mm and E (Evolving)=lesion evolution [3].
In recent years ultrasound methods have become more valid and significant in the screening diagnosis of a variety of skin tumors [2, 5, 9]. Benign and malignant skin lesions have some ultrasound characteristics that help their early and preoperative differentiation [3]. Their application in the field of maxillofacial surgery is still limited – mainly to control the growth of regional metastases [5].
The purpose of this study is to demonstrate the diagnostic abilities of multimodal 2D/3D/4D ultrasound imaging for malignant melanoma localized in the maxillofacial area in comparison to the CT, intraoperative and histologic results.
Clinical case and methods
The patient was a 39-year-old man admitted for surgery in the Department of Vascular Surgery of the Military Medical Academy because of a large painless formation in the left front half of his face. The mass caused cosmetic discomfort, but did not disturb his swallowing, speaking and breathing. Similar, but smaller formation was found in occipital area. The disease started 2-3 years earlier with the appearance of a small bump on his left temple, which gradually covered the entire front half.
The patient underwent a complex clinical examination searching for tumor formations in other locations. The brain parenchyma, cranial bones and soft tissues were evaluated by native and contrast CT of the head and neck. The major basal cerebral and facial arteries and veins were examined preoperatively with multimodal 2D/3D/4D neurosonography with B-flow imaging of the blood stream and 4-dimensional imaging of the tumor.
The big facial formation was surgically removed, fixed in 10% neutral formalin and examined histologically. Immunohistochemical methods with Vimentin, S100-protein, HMB-45, Melan A and Ki 67 were applied. Formalin-fixed composition was studied with 4-dimensional ultrasound in search of correlations with the macroscopic description of the tumor.
Results
Clinical examination
The examination found a visible facial asymmetry due to the large and irregularly shaped tumor formation involving the left side of the face (temporal, zygomatic, parotideo-masseterial and buccal areas). The mass had soft consistency and was fixed to the underlying tissues but not to the overlaying skin. Similar but substantially smaller formation (about 5 cm in diameter) was discovered in the occipital region. It had soft texture too, and no fluctuation. Both formations were painless, but the frontal one limited the active movements of the lower jaw without affecting the speech, swallowing and breathing. Enlarged regional lymph nodes and focal neurological symptoms were not detected (fig. 1).
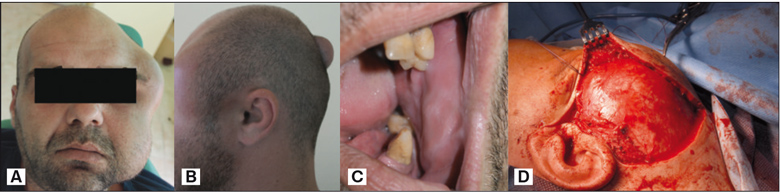
Fig. 1. Clinical view of the patient – еxtraoral view full face (А), occipital lesion (В), intraoral view (C) and intraoperative finding (D).
The examination of the nasopharynx did not establish any changes in the shape or size of structures and the lining mucosa had normal color and moisture. No suspicious pigmented lesions on the body skin were detected.
Imaging studies
Native CT scan of the head and neck performed preoperatively established normal brain parenchyma and cranial bones. A large heterogeneous tumor formation in the left facial area was displayed. It had hourglass shape above and below the zygomatic arch and was initially interpreted as lymphangioma. At the level of the lower jaw the tumor had solid structure with poor vascularization. No changes in the neighboring structures were detected. In the occipito-parietal area along the sagittal plane a second 35 mm in size formation was found. Isolated bilateral enlarged lymph nodes in the neck were present (fig. 2).
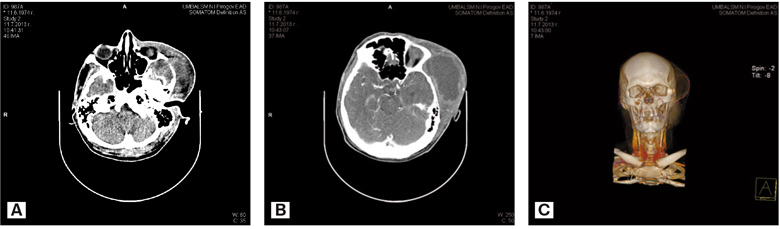
Fig. 2. CT showed a tumor formation with dense structure and sparse vascularization – native CT scan of the tumor (A), CT scan of the tumor with contrast (B), tridimensional reconstruction of the tumor lesion – expansive growth and shifting of a. temporalis superficialis were displayed (С).
Multimodal ultrasound showed a formation in the facial area with a heterogeneous structure with avascular core and well vascularized peripheral capsule. Small portions of the tumor’s caudal part were partially vascularized within the lateral segment (fig. 3). The medial part consisted of hypoechogenic zone with irregular size, anechogenic areas, lack of vascularization and formation of pseudocysts. The second formation showed predominantly homogeneous structure.
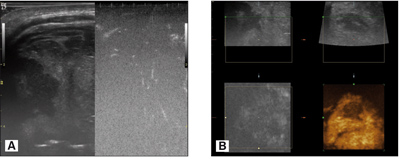
Fig. 3. The multimodal ultrasound imaging presented heterogenic structure, part of witch was less vascularlzed (A) with a distinct capsule and pseudocysts areas (B).
Intraoperatively a well encapsulated formation with expansive growth and deformed adjacent soft tissues and blood vessels were discovered (fig. 1D). The cut surface of the material showed a solid formation with presence of multiple pseudocystic areas with black color and uneven intensity.
Histopathology. Histomorphologically the tumor showed zones of deposited brown pigment and zones without pigment. In the achromatic zones the atypical cells were in nests (fig. 4A). The cells were mainly with oval and slightly elongated nucleus, with large basophilic nucleolus and abundant cytoplasm (fig. 4B).
The immunohistochemical examination of the achromatic areas proved an immunophenotype of malignant melanoma expressing Vimentin (fig. 4C), HMB 45 (fig. 4D) and Melan-A (fig. 4E). No expression of S 100 protein was detectable. This protein is not a specific marker for malignant melanoma. The tumor had moderate proliferative activity – a proliferative index Ki 67 15 (fig. 4F). In the tumor tissue multiple and extensive necroses were detectable. Part of them were with resorption and formation of pseudocysts.
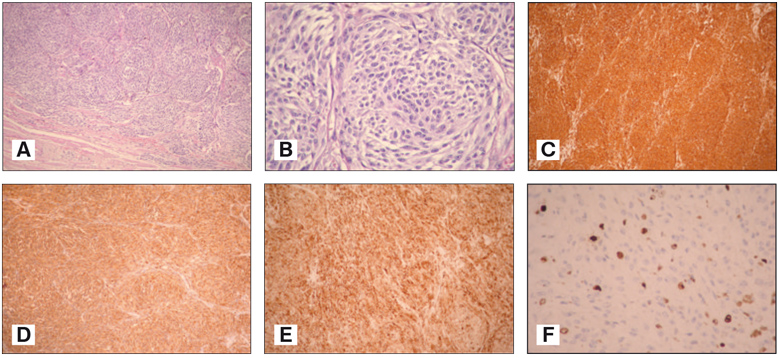
Fig. 4. Achromatic malignant melanoma with pseudoalveolar structure. Stain. H&E (A). Achromatic malignant melanoma with atypical cells with prevailing nuclei, large basophilic nucleoli and abundance of granular acidophilic cytoplasm. Stain. H&E (B). Achromatic malignant melanoma with cytoplasmic expression of Vimentin. Immunohistochemical staining (C). Achromatic malignant melanoma with cytoplasmic expression of HMB – 45. Immunohistochemical staining (D). Achromatic malignant melanoma with cytoplasmic expression of Melan - A. Immunohistochemical staining (E). Achromatic malignant melanoma with nuclear expression of Ki 67. Immunohistochemical staining (F).
The formalin-fixed tumor tissue sample was further investigated by 4-dimensional ultrasound. The sonographic findings coincided perfectly with the macroscopic description of the tissue. The pseudocysts were detected as anechogenic zones (fig. 5).
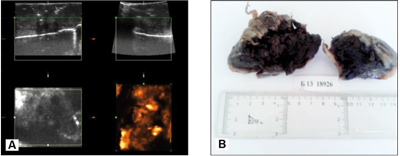
Fig. 5. Four-dimentional imaging (A) correlated with the macroscopic description of the formalin fixed tissue of the extratced tumor (D).
Discussion
This study finds a high correlation between the ultrasound imaging, CT image and macroscopic characteristics of the tumor. All three methods show a heterogeneous solid tumor with pseudocysts and distinct areas of vascularization which are nonspecific and are found in other tumors – lymphangioma, hemangioma, cysts of the soft tissues etc. Our results support the necessity of histological examination, which remains the gold standard for type differentiation of the pathological processes.
The 4-dimensional ultrasound imaging of skin lesions is not routine in clinical practice and is applied mainly for prenatal diagnosis of large tumors [6]. This study shows that the method gives more information about the structure, density, shape and volume of the formation, the presence of capsule and degree of infiltration into the surrounding tissues. The parallel use of ultrasound angiography (B-flow) objectifies the degree of vascularization of the tumor, its capsule and the surrounding tissues.
The ultrasound examination of the fixed tumor sample determines a high correlation between the macroscopic characteristics and the 4-dimensional image that justifies the use of ultrasound imaging as a navigating, noninvasive preoperative method with a similar to CT scan diagnostic value.
The localization of the tumor in the hypodermis and its good differentiation from the neighboring derma are characteristic of metastatic melanoma which in our case is with cryptogenic genesis.
In conclusion this study shows that multimodal ultrasound is a reliable diagnostic method for detection of tumors in the facial area. It provides additional information about the macroscopic structure and the vascularization of the tumor and could be used for perioperative navigation and reduction of perioperative complications. The exact diagnosis, including the histological type and biological behavior of the tumor is proved by microscopic examination and phenotyping.
REFERENCES
1. Угринов Р. Злокачествени невроектодермални тумори на кожата. В Лицево-челюстна и орална хирургия. Киви, София, 2006:501–503.
2. Aleksiev E, Guirov K, Mihova A, Guirova B, Titianova E. Clinical, intraoperative and multimodal ultrasound imaging study of facial melanoma. In: 16th World Neurosonology Meeting of the World Federation of Neurology, October 17-20, 2013, Sofia, Bulgaria. Neurosonology and Cerebral Hemodynamics 9, 2013:125–126.
3. Badea R, Crişan M, Lupşor M, Fodor L. Diagnosis and characterization of cutaneous tumors using combined ultrasonographic procedures (conventional and high resolution ultrasonography). Medical Ultrasonography 12, 2010:317–322.
4. Barnhill RL, Mihm MC Jr. The histopathology of cutaneous malignant melanoma. Semin Diagn Pathol 10, 1993:47–75.
5. Koischwitz D, Gritzmann N. Ultrasound of the neck. J. Radiologic Clinics of North America 38, 2000:1029–1045.
6. Lee S-H, Cho JY, Song MJ, Min J-Y, Han BH, Lee YH, Cho BJ, Kim SH. Prenatal Ultrasound Findings of Fetal Neoplasms. Korean J Radiol 3, 2002:64–73.
7. Neville B, Damm D, Allen C, Bouquot J. Oral and Maxillofacial Pathology, third edition, Saunders, St. Louise, Missouri, 2009: 443–439.
8. Sobin L, Gospodarowicz M, Wittekind Ch. TNM Classification of Malignant Tumours, Seventh Edition, Wiley-Blackwell, 2009, 51–53, 172–176.
9. Worstman X. Sonography of the Primary Cutaneous Melanoma: A Review. Radiology Research and Practice, 2012, www.dx.doi.org/10.1155/2012/814396.


